Zinc is a very interesting mineral. It is also one I commonly see low in hair tissue mineral analysis (HTMA).
It plays an important role in facilitating hundreds of biochemical reactions. Due to its role in enzymatic function, it can impact metabolic pathways such as carbohydrate, protein, nucleic acid, and lipid metabolism. It is also a structural component in thousands of transcription factors and can affect gene expression that impacts many physiological processes in the body. “Zinc appears to be part of more enzyme systems than all the rest of the trace minerals combined; over 300 enzymes from every enzyme class (oxidoreductases, hydrolases, lyases, isomerases, transferases, and ligases) require zinc” (Gropper, n.d.). Some of these zinc dependent enzymes include:
- Carbonic anhydrase: acid base balance- found in erythrocytes and renal tubule cells, essential for maintaining acid-base balance/buffering and respiration. The enzyme catalyzes the reaction that allows rapid disposal of carbon dioxide. Activity of this enzyme in red blood cells diminishes with chronic low zinc status in the diet.
- Alkaline phosphatase: Contains four zinc atoms per enzyme molecule, in which two are required for enzyme activity. This enzyme is found in bones and the liver.
- Alcohol dehydrogenase: contains 4 zinc molecules per enzyme molecule, two are required for catalytic activity. This enzyme is important in the NADH-dependent conversion of alcohols to aldehydes. For example, this enzyme converts retinol (form of Vitamin A) to retinal, which is needed for night vision. It also is required for acetyl aldehyde for alcohol metabolism
- Carboxypeptidases A and B and Aminopeptidases- which is involved in protein digestion. These enzymes are secreted by the pancreas into the duodenum. Zinc is bound tightly to carboxypeptidases and is essential for enzymatic activity; in fact, enzyme activity decreases with zinc deficiency (Gropper, n.d.). Aminopeptidases consist of a group of enzymes also involved in protein digestion which contains 1-2 zinc atoms for catalytic activity.
- Delta (Δ)-Aminolevulinic Acid Dehydratase: Heme Synthesis- needed for heme synthesis is zinc dependent. Interestingly, lead when present in the body in high concentrations can replace zinc in the dehydratase and diminishes heme synthesis.
- Superoxide dismutase (SOD1)- an antioxidant found in the cell cytosol requires two atoms of zinc (and two copper) to function. An extracellular form of the enzyme (SOD3) that is also zinc and copper dependent has been characterized and appears to be more sensitive to zinc than is the cytosolic form of the enzyme. Both the cytosolic and extracellular forms of superoxide dismutase serve important antioxidant defense roles in the body by catalyzing the removal of superoxide radicals, O2
- Phospholipase C-this enzyme hydrolyzes the glycerophosphate bond in phospholipids (a structural component of cell membranes!). It requires 3 zinc atoms for catalytic activity.
- Matrix Metalloproteinases-The matrix metalloproteinases are zinc containing endopeptidases (zinc is located in the catalytic site where substrate binds). They generally function in wound healing, degrading components of the extracellular matrix (among other roles) to allow for remodeling of extracellular matrix proteins and tissue repair
- Polymerases, Kinases, Nucleases, Transferases, Phosphorylases, and Transcriptases- Nucleic Acid Synthesis and Cell Replication and Growth Polymerases, kinases, nucleases, transferases, phosphorylases, and transcriptases all require zinc.
- Gene expression- Zinc plays a major structural role in regulating gene transcription by promoting a confirmation change in the shape of the transcription factor protein. You may have heard the term zinc fingers which is often used to indicate the secondary shape (configuration) of the transcription factor proteins when bound to zinc.
In addition to the above roles, zinc helps maintain cell membranes through multiple actions on membrane proteins including direct effects on membrane proteins’ conformation, on protein-to-protein interactions, and on other membrane components
Zinc itself also is believed to stabilize membrane structure by stabilizing phospholipids and thiol (SH) groups in enzymes and membrane proteins that need to be maintained in a reduced state.
Zinc may also stabilize membranes by quenching free radicals as part of metallothionein and by promoting associations between membrane skeletal and cytoskeletal proteins
Additionally, zinc in cells is found bound to tubulin, a protein that makes up the microtubules. Microtubules are thought to act as a framework for structural support of the cell as well as enable movement.
Zinc is also involved with insulin and thus influences carbohydrate metabolism. Zinc is transported into pancreatic b-cells by zinc transporter ZnT8, which also enables uptake into secretory vesicles. Pancreatic b-cells are responsible for insulin production and secretion (Gropper, n.d.).
Zinc can also influence the basal metabolic rate (BMR). A decrease in thyroid hormones and basal metabolic rate has been observed with consumption of a zinc-restricted diet (Gropper, n.d.).
Zinc is also important for taste; it is a component of gustin, a protein involved in taste acuity (Gropper, n.d.).
Cell mediated and humoral immunity are also influenced by zinc. T-cells are critical to immune system function and with zinc deficiency, thymulin activity diminishes and profoundly affects T-cell numbers and functions, and pre-T-cell apoptosis (programmed cell death) (Gropper, n.d.).
Deficiency symptoms
Some signs and symptoms of deficiency in adults include anorexia, diarrhea, lethargy, depression, skin rash/ lesions/dermatitis, hypogeusia (blunting of sense of taste), alopecia (some hair loss; remaining hair make take on a reddish hue), vision problems, and impaired immune function, protein synthesis, and wound healing (Gropper, n.d.).
Zinc deficiency can be associated with decreased mobilization of retinol from the liver (even with adequate liver vitamin A stores) as well as decreased plasma retinol-binding protein concentrations (Gropper, n.d.).
An overall deficiency of zinc stores within the body has been implicated in the systemic susceptibility of infection and in the pathogenesis of some cancers (Liu et al., 2011)
Zinc also demonstrates an important role within the lumen of the alimentary canal, as evidenced on the observations that supplementation of oral diets with Zn2+ has beneficial effects on diarrhea and inflammatory conditions of the gastrointestinal tract (Liu et al., 2011). “In gastric mucosa, adequate intracellular stores and luminal content of Zn2+ may regulate integrity of and acid secretion by the gastric glands and enhance protection of the mucosa as a whole against acid-peptic injury (Liu et al., 2011).
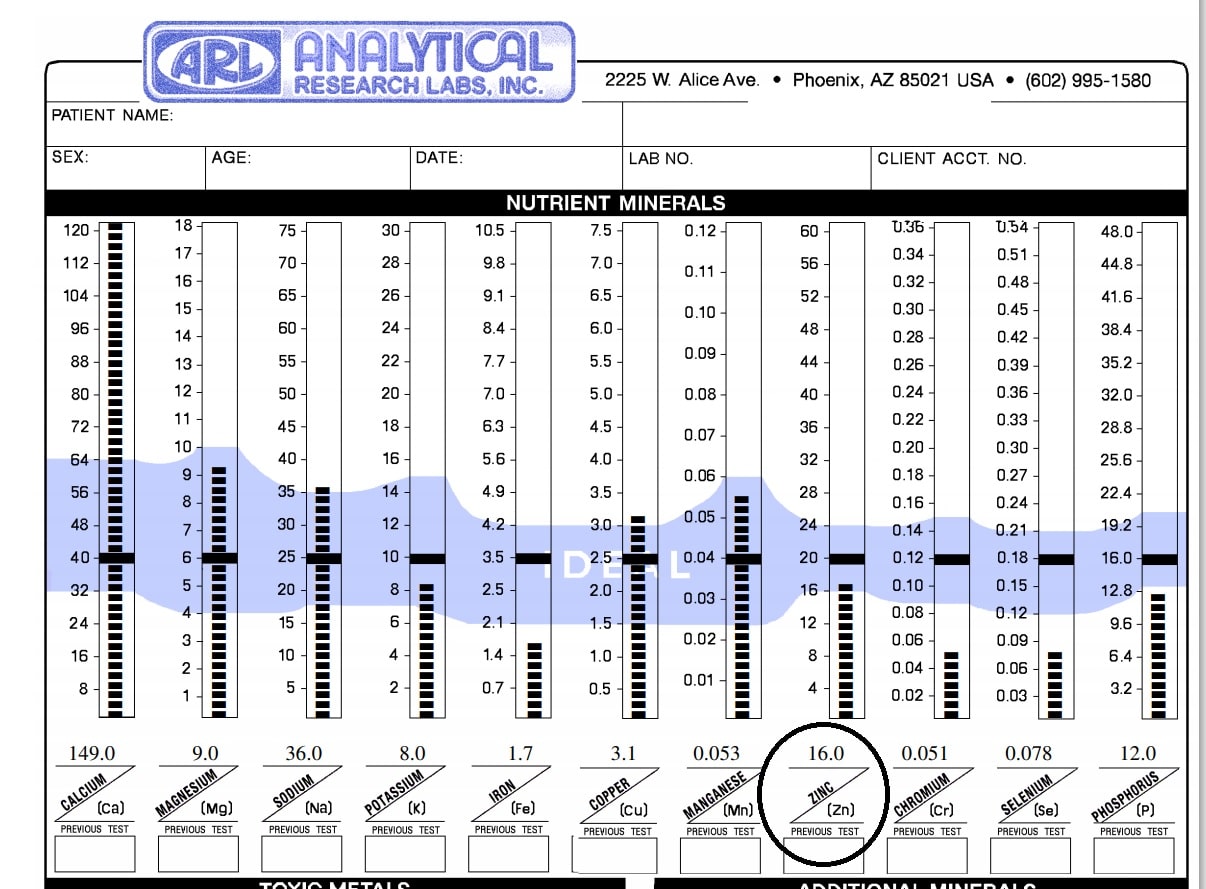
Measuring deficiency
Evaluating zinc nutriture is difficult, owing to homeostatic control of body zinc. A variety of indices have been used to assess zinc status, including measurements of zinc in red blood cells, leukocytes, neutrophils, and plasma or serum.
The most common basis for assessment is serum or plasma zinc, with fasting concentrations less than about 70 µg/dL (10 µmol/L) suggesting deficiency. A cutoff of 50 µg/dL, however, may better predict clinical signs of zinc deficiency (Gropper, n.d.). Plasma zinc concentrations range from about 70 to 120 μg/dL (10–18 µmol/L), with plasma containing about 3 mg of zinc. Plasma zinc concentrations decrease after eating, as well as under conditions of infection and trauma
Low fasting plasma zinc concentrations indicate that little zinc is present in the exchangeable zinc pool and may reflect a loss of tissue zinc (especially from the liver). Plasma zinc concentrations, however, must be interpreted with caution because concentrations are influenced by many factors unrelated to zinc depletion, including meals, time of day (diurnal variation), stress, infection, and medications such as steroid therapy. In fact, postprandial (after eating) plasma zinc concentrations have been found to be more sensitive to low dietary zinc intake than fasting plasma zinc concentrations (Gropper, n.d.)..
Metallothionein has also been used to assess zinc status. Concentrations of metallothionein respond to changes in dietary zinc. For example, liver and red blood cell metallothionein concentrations diminish as dietary zinc intake decreases and are thought to reflect zinc status or stores (Gropper, n.d.).
Serum zinc and serum metallothionein concentrations can be used to indicate poor zinc status if both are low. Elevations in serum metallothionein coupled with low serum zinc, however, usually suggest an acute-phase response, and in such conditions these indices are not reliable. Urinary zinc excretion remains fairly constant over a range of intakes and is thought to be a useful marker of status in those with moderate to severe zinc deficiency (Gropper, n.d.)..
Low hair zinc may be associated with chronic intake of dietary zinc in suboptimal amounts; however, the concentration of zinc in hair depends not only on delivery of zinc to the root but also on the rate of hair growth, which is affected by other conditions (including protein status)(Gropper, n.d.).
.Measurement of the activity of zinc-dependent enzymes has also been employed as an index of zinc status. Studies using enzymes as indicators typically have measured carbonic anhydrase or alkaline phosphatase, which “hold” zinc less securely than other zinc metalloenzymes.
Ideally, measurements of activity should be taken before and after zinc supplementation (Gropper, n.d.)..
Supplementation
Supporting deficiency in adults typically requires oral zinc supplementation; doses of 10–20 mg/day are recommended. Although higher doses (often up to 50 mg given two to three times per day) may be prescribed, use of such doses is more likely to impair copper status.
Some population groups—especially older adults, vegetarians, and those with alcoholism and with limited income—have been found to consume less than adequate amounts of zinc.
Alcohol ingestion additionally reduces intestinal zinc absorption and increases urinary zinc excretion.
Additional conditions associated with an increased need for intake include trauma, sickle-cell anemia, and disorders causing malabsorption such as Crohn’s disease, short bowel syndrome, celiac disease, and liver failure, as well as surgical bariatric procedures, especially Roux-en-Y gastric bypass and duodenal switch, used to treat obesity. Diarrhea and intestinal fistulas also substantially increase fecal zinc losses; supplementation with up to 20 mg of zinc/day may be needed under such conditions.
ZINC and COPPER
The detrimental effect of excessive zinc intake on copper absorption is thought to be attributable to zinc’s stimulation of the synthesis of metallothionein, which has a higher affinity for copper than for zinc. With increased intestinal concentrations of metallothionein induced by high zinc levels, ingested copper readily binds to the metallothionein within the enterocyte and becomes “trapped,” preventing its passage into the plasma. The increased risk of copper deficiency precipitated by zinc supplementation led to the Tolerable Upper Intake Level for elemental zinc of 40 mg daily.
Other considerations
Recent reports have begun to explore the mechanisms that regulate cellular homeostasis of Zn2+ in mucosal cells of the gastrointestinal tract (Liu et al., 2011)
There is a relationship to zinc uptake is dependent on intracellular Ca2+ stores.According to Liu et al (2011), baseline conditions, uptake of Zn2+ across the basolateral membrane depends on adequate stores of intracellular calcium ion (Ca2+) . With stimulation by powerful agonists such as forskolin and carbachol, demand for extracellular Zn2+ increases and depends on influx of extracellular Ca2+ .
“In the current set of studies, we find that Ca2+ facilitates optimal uptake of Zn2+ across the cell membrane, implying that it is either a counter-ion in exchange or it is acting as a regulatory second messenger. Membrane proteins that facilitate Zn2+ transport constitute the SLC30A (ZnT) and SLC39A (Zip) gene families” (Liu et al., 2011).
Diminished calcium absorption has been observed with the ingestion of zinc supplements when calcium intake is low (<300 mg/day of calcium). However, calcium absorption appears to be unaffected by zinc when calcium intake is at adequate (recommended) levels.
Cadmium, if present in high concentrations in the body, appears to bind to sites to which zinc would normally bind and thus disrupts normal zinc functions. For example, cadmium can replace zinc in zinc fingers, preventing the fingers from functioning as they would with zinc present.
Zinc is found in foods complexed with nucleic acids and with amino acids that are part of peptides and proteins. The zinc content of foods varies widely.
Very good sources of zinc are red meats (especially organ meats) and seafood (especially oysters and mollusks). Other relatively good animal sources of zinc include poultry, pork, and dairy products. Animal products are thought to provide 40–70% of zinc consumed by most people in the United States.
Whole grains and legumes also provide moderate amounts of zinc.
Cereals, some of which may be fortified, are thought to provide about 30% of the zinc in the U.S. diet. Fruits contain little zinc.
Plant sources, however, not only have lower zinc contents, but zinc from plants is also absorbed to a lesser extent than zinc from animal sources (e.g., meat).

Absorption
Zinc absorption is enhanced with:
Ligands or chelators including organic acids (like citric acid and picolinic acid) and prostaglandins may bind and promote zinc absorption
Glutathione and products of protein digestion, such as amino acids, serve as ligands (such as sulfur, cysteine, or nitrogen). Interestingly, amino acids serving as ligands help maintain zinc’s solubility in the gastrointestinal tract
Zinc inhibition:
Absorption of zinc is also enhanced by an acidic environment. Thus, the use of medication such as antacids, H2 receptor blockers (such as Zantac [ranitidine], Tagamet [cimetidine], or Pepcid [famotidine]), and proton pump blockers (such as Prevacid [lansoprazole] or Prilosec [omeprazole]), which are commonly taken to treat heartburn, gastroesophageal reflux disease, and ulcers, increases gastric and proximal intestinal pH and decreases zinc absorption
Phytic acid found in plant foods, particularly legumes, lentils, nuts, seeds, and whole-grain cereals decrease absorption
Other minerals such as iron and calcium negatively impact absorption
References
Gropper, Sareen S.; Smith, Jack L.; Carr, Timothy P.. Advanced Nutrition and Human Metabolism (Page 509). Wadsworth Publishing. Kindle Edition.
Liu, J., Kohler, J. E., Blass, A. L., Moncaster, J. A., Mocofanescu, A., Marcus, M. A., . . . Soybel, D. I. (2011). Demand for Zn2+ in acid-secreting gastric mucosa and its requirement for intracellular Ca2+. PLoS ONE, 6(6), e19638. doi:10.1371/journal.pone.0019638