THE ORAL MICROBIOME AND YOUR HEALTH
We talk a lot about the microbial community of the body, and thankfully, this is because even the conventional medical community is starting to recognize the importance of this community in human health. The microbiome consists of various niches such as the oral cavity, gastro-intestinal and urogenital tracts, and even the surface of your skin, to name a few. Together, these communities are referred to as your microbiome. The mouth is no exception and has its own oral microbiome (we will get to this soon).
Your microbiome is very important by the way….

Your microbiome consists of symbionts (good bacteria) and pathobionts (bad bacteria). Deviation from the symbiosis among the bacterial community leads to a condition known as “dysbiosis” or a state of community disturbance (Sudhakara, Gupta, Bhardwaj, & Wilson, 2018). When this occurs, our health can significantly be impacted.
Humans like all complex multicellular organisms are not autonomous. We are biological units that include “numerous microbial symbionts and their genomes”, and these microbes are fundamental to our health and physiology (Kilian et al., 2016). “Together with our symbiotic microbial residents, we form a ‘superorganism’, or holobiont.” As many of you know, the community of our microbial residents is referred to our “microbiome” and that includes the community in your entire body, not just your gut. “The endogenous human microbiome contributes to critical metabolic, physiological, and immunological functions including (Kilian et al., 2016)
- Differentiation and maturation of the host mucosa and its immune system
- Food digestion and nutrition
- Energy generation
- Metabolic regulation and control of fat storage
- Processing and detoxification of environmental chemicals
- Maintenance of skin and mucosa barrier function
- Development and regulation of the immune system and fine-tuning of its reaction pattern, that is, the balance between proinflammatory and anti-inflammatory processes
- Prevention of invasion and growth of disease-promoting microorganisms (colonization resistance)”
It is obvious that changes in the function and composition of the microbiome can have significant health consequences.
YOUR ORAL MICROBIOME
So let’s get to today’s topic. Let’s talk about your MOUTH.
For millions of years, our resident microbes have coevolved and coexisted with us in a mostly harmonious symbiotic relationship. The mouth houses the second most diverse microbial community in the body, with over 700 species of bacteria that colonize the hard surface of teeth and soft tissue of oral mucosa. Through recent advances in technology, we have started to understand the complexities of the oral microbiome. With metagenomic technology, we also have gained new insights into its role during both health and disease (Kilian et al., 2016).
Changes in our oral microbiome has detrimental consequences for our general oral health, and can lead to imbalanced bacterial composition otherwise known as dysbiosis. This can lead to conditions such as oral caries, gingivitis, and periodontitis to manifest (Kilian et al., 2016).
Why the focus on your mouth?
The mouth is one of the most heavily colonized parts of our bodies. It consists of two major types of bacteria in the oral microbiome: Gram-positive and Gram-negative with more than 700 species of microorganisms found in the oral cavity (Sudhakara et al., 2018). Throughout human evolution, our environment has continuously shaped the composition of our microbiome. This goes back to changes via the industrial revolution and modern eras, such as use of fire, invention of agriculture, and advent of antibiotics have all influenced the composition of the human microbiome. We have experienced a shift and decline in microbial diversity. Introduction of refined sugar in our diet caused certain bacteria to genetically evolve their metabolism to adapt to post agricultural changes in our diet. “For example, Streptococcus mutans was able to successfully compete against other oral bacterial species by developing defenses against increased oxidative stress and resistance against the acidic by-products of its own new efficient carbohydrate metabolism” (Kilian et al., 2016). This led to its increased prevalence in the oral cavity, along with other acid tolerant species in the oral microbiome.
In addition, since the industrial revolution, humans have been exposed to more toxins such as heavy metals, disinfectants, biocides, and antibiotics that have the potential to eradicate many microorganisms while positively selecting microbes that carry resistance determinants (Kilian et al., 2016).
Oral hygiene has also changed toward the end of the 19th century. Modern day excessive consumption of acidic drinks, refined sugar, alcohol and cigarette smoke has also impacted to oral ecosystem.
Recent studies have shown that several chronic conditions of the mouth and GI-tract are associated with alteration in the microbiome, which is termed as “dysbiosis”. This is defined as a significant shift in the relative abundances and individual components of the microbiome which varies with their composition and abundances during health states (Sudhakara et al., 2018). This shift can cause many common diseases we are now familiar with such as periodontitis, irritable bowel syndrome, chronic vaginosis, etc.
Biofilms
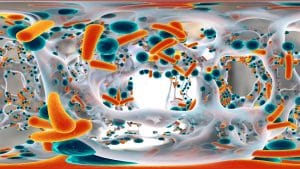
Another thing we now know is that microorganisms in our microbiome are not just unicellular organisms living alongside each other, but rather they form highly regulated, organized communities known as biofilms. This is how the microorganisms communicate with each other through a signaling process known as quorum sensing, which gives them the advantage to survive. Quorum sensing enables microorganisms in biofilms to become more tolerant to immune system defenses and antimicrobial agents.
Causes of oral dysbiosis
Poor oral hygiene is the most common cause of dysbiosis of the oral microbiome. Other major factors include dietary habits, smoking, gingival inflammation, genetics, and dysfunction of salivary glands and activity of salivary proteins. Also, as mentioned earlier, a dysbiotic shift of the microbiome imbalances in the oral microbiome can lead to the formation of biofilms. This alteration in the formation of biofilm in the oral cavity results in the accumulation of a large proportion of microbes as dental plaque biofilm. Oral dysbiosis not only causes oral related diseases, but also systemic diseases due to the manipulation of a host response.
Maintaining a healthy oral microbiome
The oral microbiome is maintained by host and microbe-derived factors. Saliva is not only involved in digestive processes, but also contain enzyme and proteins to maintain a balanced microbiota. “Up to 108 microorganisms have been detected per milliliter of saliva, mostly derived from oral mucosal surfaces such as the tongue (Kilian et al., 2016). A large number of salivary components, including secretory immunoglobulin A, lactoferrin, lactoperoxidase, lysozyme, statherin and histatins, directly and indirectly regulate the microbiome, keeping it in balance.
Another salivary component with antimicrobial potential is nitrite, converted from dietary nitrates by oral bacteria. Nitrite is further reduced to nitric oxide that can inhibit growth of cariogenic bacteria and thus may help to protect against caries. Saliva not only helps to maintain an environment that allows biofilms to flourish, but also modulates the layers of plaque with the help of numerous proteins, including enzymes and glycoproteins, and minerals, which control biofilm build-up and activity.
Your oral microbiome can even affect your heart!
Here is an interesting example of the effect how bacteria can affect your heart. We have bacteria that express an enzyme that converts nitrate from our diet to nitrite, called nitrate-reductase. After nitrite is swallowed, it is converted to nitric oxide, which is a potent vasodilator with antimicrobial activity and plays a role in regulating CV health. Nitrite also stimulates your gut mucus production. A modest consumption of nitrate has been found to lead to a reduction of blood pressure, inhibition of platelet function and reduced endothelial dysfunction. People who have an oral microbiome that favor organisms capable of nitrite reduction may have better CV function. It is now an accepted concept that the bacteria historically considered as oral ‘pathogens’ can be found in low numbers at healthy sites, and oral disease occurs as a consequence of a deleterious change to the natural balance of the microbiota rather than as a result of exogenous ‘infection’.
Disturbances in the gut microbiota by swallowed bacteria may lead to endotoxemia, caused by changes in the gut microbiota, causing metabolic disorders. The large amounts of swallowed dead bacteria from the mouth may stimulate several pathogens in the gut (called necrotrophy) and create a new phenotype by upregulation of bacterial virulence genes (called necrovirulence) and increased cytotoxicity.
Systemic consequences of oral dysbiosis
Porphyromonas gingivalis
Oral bacteria can spread throughout the body and cause systemic disease. The gut is no exception (Olsen & Yamazaki, 2019). Studies indicate that oral bacteria can translocate to the gut and change its microbiota and possible immune defense. The human subgingival plaque harbors more than 500 species of bacteria, the main player being Porphyromonas gingivalis, a Gram-negative anaerobic bacterium, is the major cause of chronic periodontitis. This strain is associated with dysbiosis in the mouth and immune defense, but also can cause dysregulation in the gut. The fact that “chronic” periodontitis may affect the gut microbiota could imply that consideration might in the future be given to a coordinated approach to the treatment of periodontitis and gastrointestinal disease (Olsen & Yamazaki, 2019). Oral bacteria can spread through the body and have been associated with a variety of systemic disease.
Enteroccocus Spp.
Another common strain I want to bring to your attention is Enteroccocus. It is a big one, as it is a common cause of urinary biofilms, UTI’s and also seen in stool tests. Enterococci are considered as transient constituent components of the oral microbiome that may cause a variety of oral and systemic infections (Komiyama et al., 2016). It is a gram-positive bacteria that inhabits the oral cavity as well as GI tract and vagina (Benbelaid et al., 2014). “It is well known that enterococci cause several infections some of which are potentially fatal, including urinary tract, neonatal and wound infections, as well as endocarditis and meningitis” (Komiyama et al., 2016). Enterococci are multidrug-resistant (MDR) bacteria to most antimicrobial drugs. This strain demonstrates the highest percentages of virulence genes as well as extracellular enzymes and a capacity to form biofilms. They suggested, therefore, that the oral cavity may constitute a critical reservoir of virulent, antibiotic resistance E. faecalis strains. In oral cavity, E. faecalis is not considered to be part of the normal oral microbiota (Benbelaid et al., 2014).
Strep spp and Candida
Molecular sequencing of the human oral cavity has demonstrated that in the supragingival plaque, S. mutans was the dominant species, with elevated levels of other streptococci including S. sanguinis, S. mitis, and S. salivarius in addition to lactobacilli and Veillonella. In contrast, the subgingival plaque was made up primarily of Gram-negative anaerobic bacteria such as Fusobacterium nucleatum, Porphyromonas gingivalis, and Prevotella intermedia which are known to be periodontal pathogens. Occurrence of disease results from disturbance of the equilibrium of this complex ecosystem, where population shifts lead to overrepresentation of pathogenic species (Metwalli, Khan, Krom, & Jabra-Rizk, 2013). What I found interesting was the association of Strep species and Candida. This drew my attention because a lot of stool tests I have seen demonstrate these two overgrown. In addition, Strep is a common urinary infection and cause of UTI, and it also can be difficult to eradicate.
Candida albicans is a commensal fungal species, commonly colonizing human mucosal surfaces. However, under conditions of immune dysfunction, Candida becomes pathogenic and opportunistic, and cause mucosal infections. Candida has the ability to switch its morphology from its yeast and hyphal form that can contribute to its pathogenesis (Metwalli et al., 2013). In the mouth, the co-adhesion between C. albicans and oral bacteria is important for C. albicans to colonize and persist. Strep excretes a fuel source (carbon) for strep, called lactate, which can provide growth stimulatory factors for Strep. Evidence indicates that the yeast cells could be used by the bacteria t support its adherence. “Scanning electron microscopic analysis of mixed species biofilms grown on human teeth and hydroxyapatite as substrata confirmed the strong coadherence between C. albicans and S. mutans to these surfaces and to each other, with S. mutans exhibiting high affinity to the C. albicans hyphae” (Metwalli et al., 2013)
Immune dysregulation in periodontitis
Often times, the host immune response is dysregulated. This can be either due to subversion by the pathogenic oral bacteria or because of defects in host immunoregulation. This can lead to bacterial overgrowth. Add to an immune response is poorly controlled, this generates a self-sustaining pathogenic cycle where dysbiosis and inflammation augment each other (Sudhakara et al., 2018). Among the immune cells, neutrophils represent the primary cellular defense in healthy oral tissues. These are the most common leukocytes recruited to the periodontal pocket and are indispensable for periodontal tissue homeostasis. Neutrophils are not very good at destroying biofilm-associated bacteria, which eventually leads to ‘frustrated phagocytosis’(Sudhakara et al., 2018). “During this process, neutrophil-derived toxic substances may also be released to the underlying tissue, causing collateral damage to tooth-supportive tissues as they function as double-edged swords, hence collateral damage can be exerted by hyperactive neutrophils or neutrophils in excessive numbers. Many bacteria, especially P. gingivalis, can subvert neutrophil functions and related immune responses causing a dysbiotic community through an impaired immune response (Sudhakara et al., 2018).
What now?
First, rule out periodontitis or any infection of your mouth. Are you going to the dentist regularly? Do your gums bleed? Do you have halitosis? Does it smell when you floss? DO you get root canals or tooth infections often? What is your hygiene like? Do you floss regularly? Better yet, do you floss and brush correctly? If you said yes to these, chances are, you have oral dysbiosis.
Next, take a look at your tongue. Your tongue is a clue to your health. Your tongue is connected to your digestive system. It can give you clues on maldigestion, malabsorption, dysbiosis, leaky gut, food allergies/intolerances and micronutrient imbalances. First thing, look at your tongue and examine:
- Color-is it pale or flaming red?
- Is there a coating, like a white coating?
- Are there any ridges on your tongue?
- What is size-is it swollen or shrunken
- Are there any lesions
- Is there anything moving on your tongue.
Some common signs include:
- Fissured tongue- could be autoimmune thyroid, leaky gut, nutrient deficiencies
- Geographic tongue- B deficiencies, food allergies, low stomach acid
- Red Beefy tongue- thyroid dysfunction, B deficiencies, folate, and others
- Coated tongue- microbial biofilm, yeast overgrowth, bacterial overgrowth
- Enlarged, scalloped tongue- food allergies, SIBO, maldigestion, nutrient deficiencies, hypothyroidism, leaky gut, toxic overload
- Bright red tongue- riboflavin deficiency, food allergy, low stomach acid, SIBO, iron deficiency, B12, B6, iron, niacin deficiency
Next, assess your stomach acid efficiency. Are you low in stomach acid? A simple HCL test can help you identify if your stomach acid production is inadequate. Here is the thing to think about: If oral bacteria can tolerate the harsh pH of the stomach, they may reside and proliferate in the gastrointestinal tract. This is particularly the case with P. gingivalis, which is acid-resistant and may migrate to the colon and change colonic functions. So don’t you think if your stomach acid production is inadequate, that can influence your ability to swallow levels of bacteria that you otherwise would not be?
And finally, test don’t guess. Run a stool, saliva and urinary test side by side. See if your urinary infections are rooted from your mouth. You may find upstream that by fixing your oral health, you may be able to fix downstream gut and bladder health as well.
What can you do about it?
Good oral hygiene is therefore crucial for controlling the total bacterial load. Good oral hygiene to control the total microbial load is important to prevent dissemination to other body sites. Treatment sessions should include prevention strategies, such as advice on oral hygiene practices and on diet and smoking. Are you using harsh mouthwash with alcohol? Do you take probiotics or use oral probiotics?
Once dysbiosis occurs, the treatment goal should be to re-establish the lost harmonious balance by keeping good oral hygiene and modifying lifestyle factors such as diet and smoking. Indiscriminate use of antibiotics for the treatment of oral diseases should be avoided, aiming to safeguard the beneficial oral microbiota and avoid antibiotic resistance. Also reduce the amount and frequency of the consumption of sucrose and acidic drinks (even sugar free) together with supplementation with agents that can reduce acid production and/ or promote alkali generation within dental plaque.
For periodontal disease, treatment strategies should aim for mechanical reduction of accumulated biofilm by mechanical removal of plaque, which means seeing your dentist 2x a year! This would reduce inflammation promote a favorable microenvironment to support formation of a balanced microbiome.
Here are my tips:
- Use xylitol toothpaste and mouthwash
- Chew xylitol gum
- Floss occasionally with tea tree oil (I dip my floss in it)
- Consider oil pulling
- Grapeseed extract and Neem are effective against Enterococcus
- Agrisept all around is helpful against Enterococcus
- Brush your tongue daily with a tongue brush
- Initiate the gag reflex with the tongue brush to activate the gut-brain axis
- Cut out the junk in your diet- but do I have to really say that? This is obvious!
- Diversify your diet with the colors of the rainbow
- Use probiotics and prebiotics appropriately. Some can cause more harm than good.
- Stay hydrated
- Use oral probiotics- some of these are really good with helping eradicate halitosis.
References
Benbelaid, F., Khadir, A., Abdoune, M. A., Bendahou, M., Muselli, A., & Costa, J. (2014). Antimicrobial activity of some essential oils against oral multidrug-resistant Enterococcus faecalis in both planktonic and biofilm state. Asian Pac J Trop Biomed, 4(6), 463-472. doi:10.12980/apjtb.4.2014c1203
Kilian, M., Chapple, I. L., Hannig, M., Marsh, P. D., Meuric, V., Pedersen, A. M., . . . Zaura, E. (2016). The oral microbiome – an update for oral healthcare professionals. Br Dent J, 221(10), 657-666. doi:10.1038/sj.bdj.2016.865
Komiyama, E. Y., Lepesqueur, L. S., Yassuda, C. G., Samaranayake, L. P., Parahitiyawa, N. B., Balducci, I., & Koga-Ito, C. Y. (2016). Enterococcus Species in the Oral Cavity: Prevalence, Virulence Factors and Antimicrobial Susceptibility. PLoS ONE, 11(9), e0163001. doi:10.1371/journal.pone.0163001
Metwalli, K. H., Khan, S. A., Krom, B. P., & Jabra-Rizk, M. A. (2013). Streptococcus mutans, Candida albicans, and the human mouth: a sticky situation. PLoS Pathog, 9(10), e1003616. doi:10.1371/journal.ppat.1003616
Olsen, I., & Yamazaki, K. (2019). Can oral bacteria affect the microbiome of the gut? J Oral Microbiol, 11(1), 1586422. doi:10.1080/20002297.2019.1586422
Sudhakara, P., Gupta, A., Bhardwaj, A., & Wilson, A. (2018). Oral Dysbiotic Communities and Their Implications in Systemic Diseases. Dent J (Basel), 6(2). doi:10.3390/dj6020010